Ankylosing Spondylitis associated with Adult Still's Disease: The First Senegalese Case Report
Moustapha Niasse1*, Awa Cheikh Ndao2, Ramadhane Bouchrane1, Siddiki Charifah1, Adama Bah1, Saïdou Diallo1
1Department of Rheumatology, University Hospital Aristide Le Dantec of Dakar, Senegal
2Department of Internal Medicine, University Hospital Aristide Le Dantec of Dakar, Senegal
Introduction
Ankylosing spondylitis is the most common type of spondyloarthritis1, a group of diseases characterized by axial skeleton and sacroiliac involvement, peripheral joints and/or entheseal involvement and extra-articular manifestations1,2. Other types of spondyloarthritis are psoriatic arthritis, reactive arthritis, arthritis associated with cryptogenetic inflammatory bowel disease, S.A.P.H.O. (Synovitis, Acne, Pustulosis, Hyperostosis and Osteitis), juvenile spondyloarthritis and undifferentiated forms. All other forms of spondyloarthritis can develop into ankylosing spondylitis1,2. This form, which can also occur at the outset, is characterized by the presence of sacroiliitis, often associated with stiffness and spinal deformities1,2,3.
General signs such as fever are rarely found in ankylosing spondylitis4. Their existence is often linked to the association of other diseases, notably infectious diseases or other types of auto-inflammatory diseases, including adult Still's disease. It is characterized by a triad of constant hectic fever, skin rash and arthritis and other miscellaneous manifestations6. The association between ankylosing spondylitis and adult Still's disease is rarely reported in the literature5. We report the first case in Senegal.
Case Report
A 43-year-old man followed up since April 2019 for ankylosing spondylitis diagnosed in accordance with the ASAS and modified New York criteria7,8. He presented a radiographic axial form with bilateral stage 3 sacroiliitis (Figure 1), associated with enthesitic peripheral involvement (bilateral plantar talalgia). HLA-B27 antigen was positive. Ankylosing spondylitis was active with a BASDAI of 45/100 and an ASDAS-CRP of 3.26. The patient was treated with non-steroidal anti-inflammatory drugs and methotrexate (15 mg per week); which is indicated in front of the peripheral attacks of spondyloarthritis. Evolution was marked by remission after three months of treatment.
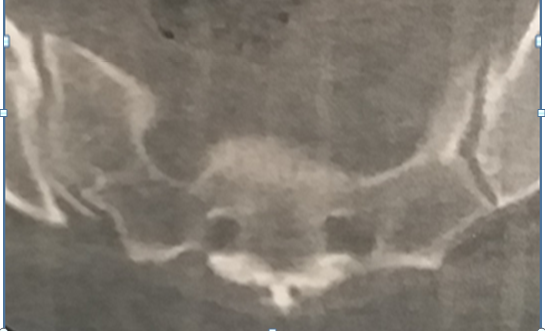
Figure 1: CT image showing bilateral sacroiliitis in our patient. We note diffuse sclerosis and irregular erosions of the sacroiliac joints giving « a postage stamp » appearance.
In January 2020, he suddenly presented with a hectic fever oscillating between 38 and 39°5 c associated with peripheral, bilateral asymmetric polyarthritis involving the left knee, the right wrist and both ankles. The patient also complained of odynophagia, prompting ENT examination which revealed a non-exudative pharyngitis. The examination did not reveal any skin rash. Biological workup showed an inflammatory syndrome with an erythrocyte sedimentation rate of 82 mm at the first hour and a C-reactive protein of 212 mg/l.
Complete blood count showed hyperleukocytosis (14,000 leukocytes/mm3) with neutrophil predominance (85%), normochromic normocytic anaemia with a haemoglobin level of 9 g/dl and a normal platelet count (420,000/mm3). Aspartate amino transferase values were elevated at 51 IU/l and alanine amino transferase was normal at 37 IU/l. There was hyperferritinemia at 10 times normal levels (1587 ng/ml).
The glycosylated fraction was reduced (10%). Infectious tests were negative. These included thick blood drop, blood cultures, throat swabs, urine cultures, viral serology tests (hepatitis B, hepatitis C and HIV) and syphilis. Immunological tests including rheumatoid factor, anti-cyclic citrullinated peptide antibodies and antinuclear antibodies were also negative. The diagnosis of adult-onset Still's disease (AOSD) was thus made in accordance with the criteria of Fautrel9, and with those of Yamaguchi10. Non-steroidal anti-inflammatory drug was replaced by prednisone 1 mg/kg/day. Methotrexate, which was still being used before the onset of Still's disease, was continued. The course of treatment was favourable, with gradual reduction of the corticosteroids after 4 weeks.
Commentary
Ankylosing spondylitis is a chronic inflammatory rheumatic disease in which fever is rarely present4. Thus, the presence of fever suggests its association with other febrile conditions5. In our case, ankylosing spondylitis was associated with adult-onset Still's disease, which caused fever at nine months of follow-up.
The association of these two conditions suggests a coincidence or a pathophysiological link5. Indeed, both diseases are classified in the group of polygenic auto-inflammatory pathologies11,12 which are mediated by innate immunity with a high production of pro-inflammatory cytokines (IL-1 β, IL-18, IL-6 and TNF-α). IL-1β, and IL-18 are activated by caspase-1, which is the main effector protease of the inflammasome13,14.
Nonetheless, despite the pathophysiological links, the association between ankylosing spondylitis and adult Still's disease is rarely reported5,15. However, this rarity may reflect an underestimation, especially as Cush found sacroiliitis in 9.1% of adult Still's disease in a large review of articles16. To the best of our knowledge, between 2000 and 2020, eight (8) cases of this association in four (4) studies were published (see table, below).
These cases, as ours, all concerned men. Spondyloarthritis, as in our case, had preceded adult Still's disease. The types of spondyloarthritis were: ankylosing spondylitis (5 cases), psoriatic arthritis (2 cases) and undifferentiated spondyloarthritis (1 case). Psoriatic arthritis was found in a 21-year-old man and in his father. Our case is about a 43 years old who presented with ankylosing spondylitis. The average age of the 8 patients was 40 years (extremes: 21 and 62 years), similar to that of our patient (43 years). In adult Still's disease, fever and arthralgia were constant in all patients (Table 1).
Table 1:Comparing the characteristics of 8 reported cases in literature of the association Spondyloarthritis and adult Still’s disease to those of our patient
|
Authors |
Maeda H, et al. [17] |
Akkoc N, et al. [15] |
Aradoini N, et al. [5] |
Duran TI, et al. [18] |
Our case |
|
Country |
China |
Turkey |
Morocco |
Turkey |
Senegal |
|
Year |
2000 |
2008 |
2017 |
2020 |
2021 |
|
Number of cases |
2 |
4 |
1 |
1 |
1 |
|
Age (in years) |
Case 1 : 21 Case 2 : 46 |
N.F |
31 |
62 |
43 |
|
Types of spondyloarthritis |
Psoriatic arthritis : 2 |
A.S: 3 Undifferentiated Spondyloarthritis : 1 |
A.S : 1 |
A.S : 1 |
A.S : 1 |
|
Presence of HLA-B27 |
N.F |
N.F |
N.F |
N.F |
Oui |
|
Delay between spondyloarthritis and adult Still's disease onset |
Case 1 : 4 years Case 2 : 4 years |
N.F |
10 years |
15 years |
9 months |
|
Fever |
40°C |
High (N.Q) |
40°C |
Oui (N.Q) |
38-39,5°C |
|
Skin rash |
Absent |
Present |
Present |
Absent |
Absent |
|
Arthritis |
Present |
Present |
Present |
Present |
Present |
|
Odynophagia |
Case 1: Present Case 2: N.F |
3 of the 4 cases |
N.F |
Present |
Present |
|
Organomegaly |
Case 1: Present Case 2: N.F |
N.F |
Present |
Present |
Absent |
|
Leukocytes/mm3 |
Case 1: 13800 Case 2: 10300 |
N.F |
15000 |
11650 |
14000 |
|
C-reactive protein (mg/l) |
Case 1: 12,5 Case 2: 3,4 |
High (N.Q) |
300 |
192 |
212 |
|
Ferritinemia (ng/ml) |
Case 1: 4 N Case 2: N.F |
N.F |
31 N |
9 N |
10 N |
|
Glycosylated fraction |
N.F |
N.F |
15% |
N.F |
10% |
|
Rheumatoid factor |
Negative |
Negative |
Negative |
Negative |
Negative |
|
Antinuclear antibodies |
Negative |
Negative |
Negative |
Negative |
Negative |
|
Infectious tests |
Negative |
Negative |
Negative |
Negative |
Negative |
N.F: not filled in ; N.Q: not quantified; A.S : Ankylosing spondylitis ; N : normal
Skin rash was present in 6 cases. On the biological level, the C-reactive protein was highly elevated except in 1 case, in which it was normal17. Hyperleukocytosis was noted in 6 cases. Ferritin levels in 4 patients, including our patient, were between 4 and 31 times normal. The glycosylated fraction was measured in our patient and in Aradoini5. It was collapsed (<20%) in both cases. The values were 10% and 15% respectively. The immunological tests, as well as infection workups, were negative in all cases.
Treatment of our patient is in accordance with the literature. Indeed, in spondyloarthritis, non-steroidal anti-inflammatory drugs are used as first line treatment and in adult Still's disease, high dose corticosteroids are indicated as first line treatment12. These anti-inflammatory treatments are often combined with conventional disease-modifying antirheumatic drugs (DMARDs)18.
The use of DMARDs has anti-inflammatory drug sparing effect. Thus, in our patient, the maintenance of methotrexate allowed an early reduction of the corticosteroid dose after 4 weeks of treatment.
Conclusion
Our observation indicates the existence of the association between ankylosing spondylitis and adult Still's disease in our context. Thus, the association is certainly rare but possible. This couple must be evoked each time a known patient with spondyloarthritis presents a fever with a significant biological inflammatory syndrome and hyperleukocytosis with neutrophil predominance, after infectious and neoplastic diseases have been ruled out.
Conflict of Interest
The authors have no conflicts of interest.
References
- Cotten A, Philippe P, Flipo R-M. Spondyloarthritis. Imagerie musculo-squelettique: Pathologies Générales (2e édition) 2013, Elsevier Masson SAS, p: 137-187.
- Claudepierre P, Wendling D. Ankylosing spondyloarthritis. EMC (Elsevier Masson SAS, Paris), Appareil locomoteur, 14-230-A-10, 2009.
- Mangone M, Paoloni M, Procopio S, et al. Sagittal spinal alignment in patients with ankylosing spondylitis by rasterstereographic back shape analysis: an observational retrospective study. Eur J Phys Rehabil Med. 2020; 56(2): 191-196.
- Alert JB, Gentelle S, Grasland A, et al. The febrile forms of ankylosing spondylitis. Revue de Médecine Interne. 2002; 23: 81-84.
- Aradoini N, Talbi S, Azzouzi H, et al. Ankylosing spondylitis and Still's disease: a pathophysiological link or just an association? Pan African Medical Journal. 2017; 28: 132.
- Ribi C. Still's disease in adults. Revue Médicale Suisse. 2008; 4: 1039-1044.
- Rudwaleit M, van der Heijde D, Landewé R, et al. The Assessment of Spondyloarthritis International Society classification criteria for peripheral spondyloarthritis and for spondyloarthritis in general. Annale Rheumatic Disease. 2001; 70: 25-31.
- Van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum. 1984; 27(4): 361-8.
- Fautrel B, Zing E, Golmard JL, et al. Proposal for a new set of classification criteria for adult-onset Still disease. Medecine. 2002; 81: 194-200.
- Yamaguchi M, Ohla A, Tsunematsu T, et al. Preliminary criteria for classification of adult Still’s disease. The Journal of Rheumatology 1992; 19: 424-430.
- Jamilloux Y, Sève P, Henry T. Inflammasomes and human diseases. Revue de Médecine Interne. 2014; 35: 730-741.
- Wahb M, Rachidi W, Nassar K, et al. Adult Still's disease: therapeutic update. Revue Marocaine de Rhumatologie. 2015; 32: 32-38.
- Gerfaud-Valentin M, Sève P, Hot A, et al. Updated data on the pathophysiology, phenotypes and treatments of adult Still's disease. Revue de médecine Interne. 2015; 36: 319-327.
- Fauter M, Gerfaud-Valentin M, Delplanque M, et al. Complications of adult Still's disease. Revue de Médecine Interne. 2020; 41: 168-179.
- Akkoc N, Sari I, Birlik M, et al. Ankylosing spondylitis and spondyloarthropathy presenting with a clinical picture of adulte onset Still’s disease: case series. Rheumatology (Oxford). 2008; 47(9): 1436-1437.
- Cush JJ. Adult-onset Still’s disease-a circadien cytokine syndrome? Journal Medicine Grand Rounds. The University of Texas Southwestern Medical Center at Dallas. 5 January 1994; Accessed on August 20, 2019.
- Maeda H, Konishi F, Hiyama K, et al. A Family with Cases of Adult Onset Still’s Disease and Psoriasic Arthritis. Internal Medicine. 2000; 39: 77-79.
- Duran TI, Kehribar DY, Ozgen M. Adult-onset Still’s Disease Detected in Ankylosing Spondylitis Patient using Adalimumab. Journal of college of physicians and surgeons Pakistan. 2020; 30(12): 1364.
