Geographic Distribution of Inflammatory Breast Cancer and Non-Inflammatory Breast Cancer in Gharbiah, Egypt
An Nguyen1, Amr S. Soliman2*, Ahmed Hablas3, Mohamed Ramadan3, Ibrahim Seifeldin3
1Milken Institute School of Public Health, The George Washington University, Washington, DC, USA
2CUNY School of Medicine, New York, NY, USA
3Gharbiah Cancer Society, Tanta, Gharbiah, Egypt
Abstract
BACKGROUND: Inflammatory Breast Cancer (IBC) is a rare but aggressive form of breast cancer, constituting about 1-5% of breast cancers in the U.S. but about 11% in Egypt. The etiology of IBC is unknown, but the distribution of residence of IBC and non-IBC patients may provide clues to the disease risk factors. Therefore, we investigated the geographic distribution of IBC and non-IBC in the province of Gharbiah, Egypt.
METHODS: All breast cancers diagnosed during the period of January 2009 to December 2010 were retrieved from the Gharbiah Population-based registry. IBC cases were obtained from a case-control study conducted in the same region and period. Incidence rates were calculated for IBC and non-IBC for each of the eight districts and their rural/urban regions.
RESULTS: The incidence of IBC was higher in rural than urban areas, in contrast to the incidence of non-IBC. Clustering of IBC and non-IBC was observed more in urban than in rural areas. IBC clusters were detected in 7 of the 8 urban areas of Gharbiah, with the highest incidence identified in urban Kafr El-Zayat. Non-IBC clusters were distributed in all 8 urban areas of Gharbiah without clustering, with highest incidence is identified in urban Tanta.
CONCLUSION: Our results showed different geospatial distributions of IBC and non-IBC relative to the regional environmental exposures. Future studies should explore specific environmental exposures that may contribute to the geographic distribution of IBC and non-IBC in the region to further explore the etiology of IBC and non-IBC.
Introduction
Breast cancer is one of the three most common cancers worldwide, along with lung and colon cancers1. Although breast cancer incidence rate is higher in developing than developed countries, the relative mortality rate of the disease is greater in developing countries, including those in South America, North and East Africa, and South-East Asia2. Breast cancer is the most common cause of cancer mortality in low- and middle-income countries (LMICs).
Inflammatory breast cancer (IBC) is a rare but the most aggressive form of breast cancer. IBC accounts for 1 to 5% of all breast cancers diagnosed in the United States3,4. Compared to other types of breast cancer, IBC tends to be diagnosed at a younger age and more common in African American women than other racial groups4-8. Previous studies showed a high proportion of IBC in North Africa with approximately 6% in Tunisia, 5% in Morocco and 11% in Egypt7,9-10. Little is known about the etiology of IBC4,8. Although a study evaluated the spatial incidence of IBC from 2004 to 2012 in the U.S and confirmed that IBC rates differed geographically and may be influenced by socioeconomic and environmental factors,11 no studies have investigated IBC distribution in low- and middle-income countries. While the proportion of IBC to all breast cancers in North Africa is higher than other international regions and a wide range of environmental exposures and socioeconomic levels exit, no studies have explored the geographic distribution of IBC in this region. Therefore, using a well-validated population-based cancer registry data2 and an epidemiologic research study,12,13 we conducted this study to explore the geographic distribution of IBC in comparison to non-IBC in Egypt.
Methods
Study Settings and Population - This study included 2 groups of cases: a group of IBC cases from a well-characterized epidemiologic case-control study,12,13 and a group of non-IBC cases from the Gharbiah Population-Based Cancer Registry (GPCR)2. All IBC and non-IBC cases were diagnosed from January 2009 to December 2010. All 65 female IBC cases were obtained from the Gharbiah Cancer Society (GCS) and Tanta Cancer Center (TCC) and their clinical diagnosis was confirmed in our previous study12. All 1,680 female non-IBC cases were obtained from the GPCR that is based on active registration and validation of all cancer cases of the province2. All non- IBC breast cancer cases obtained from the registry were classified based on the World Health Organization’s ICD-O-3 coding for 2001 onward,14 including C.50, C50.1, C.50.2, C.50.3, C.50.4, C.50.5, C.50.6, C.50.8, and C.50.9. IBC cases were identified based on the standard clinical diagnostic criteria of the disease13. After removing all personal identifiers, information that was retained for the statistical analysis included age at diagnosis, number of children, and district and urban/rural place of residence. The study was approved by the Gharbiah Cancer Society’s Ethics Committee and the George Washington University’s Institutional Review Board.
Data Management and Statistical Analyses
Data Management
Census Data and Incidence Rate – Census data of the female population of all age groups in urban cities and rural villages in the 8 districts of Gharbiah were obtained from the Egyptian Central Agency for Public Mobilization and Statistics (CAPMAS, 2006)15. Based on these data, the Annual Growth Rate (AGR) of the population was calculated using the following formula: AGR =
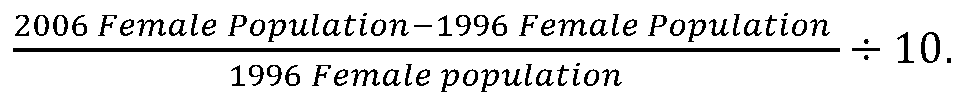
The calculated growth rate (1.8%) was then used as a multiplication factor to estimate the yearly female populations of the province and of each district. The population estimates were then used as the denominators for calculating crude incidence rates of IBC and non-IBC of each urban/rural area of all districts. CAPMAS classified agricultural areas as rural whereas cities are urban areas (CAPMAS, 2006)15.
The available data did not allow us to identify breast cancer cases in both urban and rural areas of El-Santa, Samanoud, and Kotour districts during the study period. Therefore, we excluded breast cancer cases that were diagnosed in only rural places of residence from these specific districts from our statistical analyses and comparisons.
Statistical Analysis
Summary statistics, unadjusted odds ratios (ORs), and rural/urban crude incidence rates (IR) with statistical significance for each district were computed using SAS Software (9.14. SAS Institute Inc., Cary, NC, USA). To compare urban and rural incidence rates of each district, the corresponding incidence rate ratios (IRRs) were also computed using Microsoft Excel (16.29.1. 2019 Microsoft).
Results
A total of 1,750 breast cancer cases (65 IBC cases and 1,685 non-IBC cases) from 2009 to 2010 were obtained from the GPCR (Table 1). Our data showed significantly higher odds of developing IBC among women who were in the 15-to-34 age group (OR=3.2, p=0.006, 95% CI: 1.39,7.25) and among those who had 4 to 6 children (OR=2.3, p=0.02, 95% CI: 1.13,4.75).
Table 1: Characteristics of 65 Female IBC and 1,685 Female non-IBC Patients in Gharbiah Province (2009-2010).
|
Variables |
Total BC |
IBC (n = 65) |
Non-IBC (n = 1,685) |
p-value |
Unadjusted OR (95% CI) |
|
Age at Diagnosis n (%)
15-34 years old 35-44 years old 45-54 years old 55-64 years old 65-74 years old 75+ years old
|
123 349 553 472 181 72
|
10 (15.40) 14 (21.50) 15 (23.10 13 (20.00) 10 (15.40) 3 (4.60) |
113 (6.70) 335 (19.90) 538 (31.90) 459 (27.20) 171 (10.10) 69 (4.10)
|
0.006 0.28 Ref. 0.9 0.07 0.5 |
3.2 (1.39, 7.25) 1.5 (0.71, 3.15) Ref. 1.0 (0.48, 2.16) 2.1 (0.92, 4.75) 1.6 (0.44, 5.52)
|
|
Number of Children n (%)
0 1-3 4-6 7-9 Unknown
Missing value = 5
|
396 (22.69) 590 (33.81) 419 (24.01) 57 (3.27) 283 (16.22)
|
11 (16.92) 25 (38.46) 26 (40.00) 3 (4.62) 0 (0.00)
|
385 (22.92) 565 (33.63) 393 (23.39) 54 (3.21) 283 (16.85)
|
Ref. 0.23 0.02 0.32 - |
Ref. 1.55 (0.75, 3.18) 2.31 (1.13, 4.75) 1.94 (0.53, 7.19) -
|
|
Place of Residence n (%)
Urban Rural
Missing value = 1
|
918 (52.49) 831 (47.51)
|
26 (40.00) 39 (60.00)
|
892 (52.97) 792 (47.03)
|
0.04 Ref. |
0.60 (0.36, 0.98) Ref.
|
Overall, this study revealed that the odds of developing IBC and non-IBC among female residents of Gharbiah province were not uniformly observed across the 8 districts (Table 2). When comparing urban versus rural places of residence of the province, our data showed a significant decrease in the odds of having IBC among urban cases (OR=0.60, p=0.02, 95%CI: 0.36, 0.98) compared to non-IBC cases. On the urban-rural scale within each district, although the odds of developing IBC were higher in Mehalla, Kafr Elzayat, Basyoun, and Zefta districts, these results were not statistically significant. However, we found that urban women of Tanta district had significantly lower odds of developing IBC (OR=0.30, p=0.0007, 95%CI: 0.14, 0.62) as compared to rural women living in the same district (Table 2).
Table 2: Unadjusted odds ratios of breast cancers in women living in urban versus rural places of residence in Gharbiah Province, Egypt.
|
|
IBC n (%) |
Non-IBC n (%) |
p-value for Fisher test for IBC vs. non-IBC |
Unadjusted OR (95% CI)
|
|
All Gharbiah
Urban Rural
Missing value = 1
|
65
26 (2.8) 39 (4.7)
|
1684
892 (97.2) 792 (95.3) |
0.04
|
0.60 (0.36, 0.98) Ref. |
|
Tanta
Urban Rural |
34
12 (3.3) 22 (10.4)
|
536
346 (96.7) 190 (89.6) |
0.0007 |
0.30 (0.14, 0.62)
|
|
Kafr El-Zayat
Urban Rural |
5
4 (5.9) 1 (1.2)
|
143
64 (94.1) 79 (98.8) |
0.14 |
4.94 (0.54, 45.3) |
|
Mehalla El-Kubra
Urban Rural
|
10
7 (2.0) 3 (2.0) |
490
344 (98.0) 146 (98.0) |
0.65 |
0.99 (0.22, 6.01) |
|
Kotour
Urban Rural
|
3
0 3 (4.1)
|
79
9 (100.0) 70 (95.9) |
0.70 |
n/a |
|
Basyoun
Urban Rural |
3
2 (8.0) 1 (1.4)
|
95
23 (92.0) 72 (98.6) |
0.16 |
6.26 (0.54, 72.2) |
|
Zefta
Urban Rural
|
2
1 (1.6) 1 (1.3) |
139
61 (98.4) 78 (98.7) |
0.69 |
1.28 (0.07, 20.8) |
|
Samanoud
Urban Rural |
3
0 3 (4.6)
|
83
21 (100.0) 62 (95.4) |
0.43 |
n/a |
|
El Santa
Urban Rural
|
5
0 5 (5.0) |
119
24 (100.0) 95 (95.0) |
0.33 |
n/a |
Table 3 presents the crude incidence rates for urban and/or rural areas of all eight districts, together with the urban-rural incidence rate ratios of five districts (El Santa, Samanoud, and Kotour were excluded). Incidence rates for IBC were higher in urban areas of Mehalla, Kafr Elzayat, Basyoun, and Zefta (2.93, 10.47, 7.16, and 2.02 per 100,000; respectively), except for urban areas of Tanta district (5.28 per 100,000). Incidence rates for non-IBC were consistently higher in urban areas of all five districts of Gharbiah province, including Tanta, Mehalla, Kafr Elzayat, Basyoun, and Zefta (152.24, 143.78, 167.50, 82.32, and 123.27 per 100,000; respectively). Only four districts of Gharbiah province show high urban-rural incidence rate ratios (IRRs) of IBC, whereas all five districts included in the analysis of this study consistently show high urban-rural IRRs of non-IBC. Figure 1 illustrates the relative locations of all eight districts of Gharbiah province (Table 3).
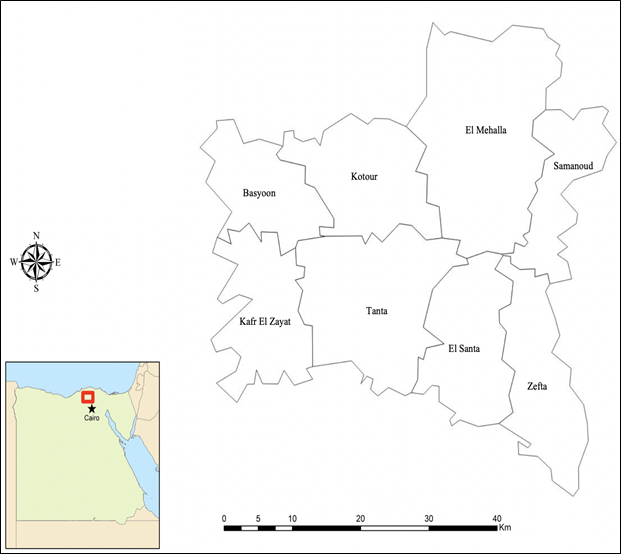
Figure 1: Regional map of all eight districts of Gharbiah Province.
Table 3: Crude incidence rates (IR) and urban-rural incidence rate ratios (IRR) of 65 IBC and 1,684 non-IBC cases in Gharbiah Province (2009-2010).
|
Urban/Rural Residence |
IBC Count |
Non-IBC Count |
Crude IR of IBC (per 100,000) |
Urban-Rural IRR of IBC |
Crude IR of non-IBC (per 100,000) |
Urban-Rural of IRR of non-IBC |
|
Urban Tanta |
12 |
346 |
5.28 |
0.68 |
152.24 |
2.27 |
|
Rural Tanta |
22 |
190 |
7.77 |
67.13 |
||
|
Urban Mehalla |
7 |
344 |
2.93 |
3.05 |
143.78 |
3.07
|
|
Rural Mehalla |
3 |
146 |
0.96 |
46.82 |
||
|
Urban Kafr Elzayat |
4 |
64 |
10.47 |
16.90 |
167.50 |
3.44 |
|
Rural Kafr Elzayat |
1 |
79 |
0.62 |
48.64 |
||
|
Urban Basyoun |
2 |
23 |
7.16 |
7.09 |
82.32 |
1.13 |
|
Rural Basyoun |
1 |
72 |
1.01 |
72.59 |
||
|
Urban Zefta |
1 |
61 |
2.02 |
3.74 |
123.27 |
2.90 |
|
Rural Zefta |
1 |
78 |
0.54 |
42.07 |
||
|
Rural Elsanta |
6 |
119 |
3.34 |
n/a |
66.33 |
n/a |
|
Rural Samanoud |
3 |
83 |
2.33 |
n/a |
64.39 |
n/a |
|
Rural Kotour |
2 |
79 |
1.49 |
n/a |
58.99 |
n/a |
|
Total |
65 |
1,684 |
3.14 |
|
81.50 |
|
Discussion
Our study revealed a few interesting observations. First, this study showed both IBC and non-IBC rates were not uniformly distributed across all the districts of Gharbiah, which is consistent with previous finding of breast cancer clusters in the U.S. and in Egypt11,17. Although socioeconomic status (SES) may be the most crucial risk factor of breast cancer, in addition to many additional factors, including breast cancer screening, transportation, housing quality and living conditions etc.,11 in our Egyptian study population in Gharbiah, poverty may not affect the rates of low breast cancer diagnosis as there is no major difference in SES within the province17,18. Also, there are no programs for early detection or screening for breast cancer across the different parts of the province.
Second, different urban-rural geographic patterns of IBC were observed in five districts of the province (i.e., Tanta, Kafr El-Zayat, Basyoun, El Mehalla, and Zefta). Compared to the other districts, only Tanta showed both lower odds ratios and lower incidence rate ratio of IBC in urban areas. All the four remaining districts consistently showed higher incidence rate ratios of IBC in urban compared to rural places of residence, which opposed the observation of rural predominance of IBC in Tunisia6,16. This could be due to the fact that rural Tanta women have been increasingly adopting urban lifestyles and that their reproductive habits have changed over time as a result of rapid economic development and urbanization in Tanta17,18.
Third, higher non-IBC rate ratios were observed in all 5 urban areas of the Gharbiah province. These findings were expected because previous study investigating breast cancer trends in Egypt also showed higher incidence of breast cancer in urban than in rural areas of Gharbiah province17,18. In addition, previous studies in Egypt discovered that not only did urban Egyptian women have higher levels of carcinogen (i.e. 7,8-dihydro-8-oxo-2’-deosyguanine (8-oxo-dG),19 but they might also have been exposed dangerously high levels of heavy metals and inorganic pollutants urban areas of Gharbiah20,21.
Finally, this study showed that urban Kafr El-Zayat had the highest incidence rate ratios of both IBC and non-IBC, suggesting a possible association between these two subtypes of breast cancer and high exposure levels of heavy metals and inorganic pollutants in Kafr El-Zayat district22-25. While Kafr El-Zayat is not the most populated and urbanized city of the province, it is home to pesticide factories, agricultural activities, soap, sewage disposal sites, industrial-related wastewater management, and textiles. Therefore, we speculate that women in the district may experience greater exposure to environmental risk factors such as xenoestrogens and heavy metal contamination, which may contribute to the highest ranks and consistent patterns of both IBC and non-IBC rates.
Rural-urban classification and exposures in Egypt are different from those in a developed country, such as the U.S. The rural-urban classification in Egypt is based on the occupations of residents. Villages, where agriculture/farming is the primary occupation are classified as rural while cities in which occupations are non-agricultural are classified as urban. This is the official classification of the Egyptian government defined by the Central Agency for Public Mobilization and Statistics (CAPMUS), the governmental agency responsible for the Egyptian census, population statistics, and demographic data15. This has been the classification that was used by the Gharbiah population-based cancer registry. In the United States, rural-urban classification is defined based on the continuum codes (RUCC). For example, codes 1-3 refer to metro counties (1 million to <250,000 people), while codes 4-9 refer to non-metro counties, including rural areas (>20,000 people and adjacent to a metro area, or <2,500 people and not adjacent to a metro area26. In addition to the different methods of rural-urban classification, the levels of environmental exposures are also different between countries. For example, due to the lack of environmental regulations at the federal and local levels in Egypt, exposures to industrial pollution in Egypt are higher due lack of enforcement of environmental protection laws27.
We suspected that the rapid economic development and urbanization in Tanta has shifted the urban-rural geographic pattern of IBC in the district. More rural Tanta women have increasingly exhibited exposures similar to exposures in urban Tanta. In addition, rural Tanta women have become more educated and gradually adopted urban lifestyles (e.g., obesity, energy-dense diet, and fast food) and urban reproductive habits (e.g., more contraceptive use, older age at first child-birth, fewer children, and shorter duration of breastfeeding.
Although Gharbiah residents have been predominantly participating in agricultural activities (e.g., cotton cultivation and production), they are also exposed to other sources of environmental pollution. For examples, the Gharbiah province has one of the largest pesticide factories in Kafr ElZayat district, as well as the country’s largest textile factory in Mehalla district. We suspect the variable agricultural and industrial exposures in the region are the main factors leading to the lack of uniformity of IBC and non-IBC in the province.
The main strength of this study was the high-quality data of validating of IBC diagnoses by committees of experts in Egypt and the U.S., as needed for the case-control study12,13. Non-IBC cases were also well-characterized and validated in the Gharbiah Population-Based Cancer Registry2. In addition, our study used well-characterized data of the Egyptian census data from CAPMAS. Furthermore, due to the lack of SES differences in our Egyptian population, our findings allow future studies to focus on environmental risk factors.
The relatively short period of the study is a limitation. It is possible that the rates may not be stable enough to determine the trend of IBC incidence in Gharbiah. Specifically, our findings did not entirely support findings from previous studies that were also conducted in the same region yet showed higher incidence of breast cancers in urban than rural places of residence17,18. Thus, the geographic distribution patterns of IBC seen from 2009-2010 from this study may not reflect the long-term IBC incidence patterns in Gharbiah province. Another limitation in our study was that non-IBC data obtained from the population-based cancer registry (GPCR) did not provide individual level information on the risk factors which restricted our ability to make the definite link between environmental links to the distinct and consistent urban/rural patterns of non-IBC. However, a population-based cancer registry is not designed to collect environmental or exposure risk factors.
In conclusion, this study explored the geographic distribution of breast cancer in Gharbiah province of Egypt to define patterns of IBC and non-IBC and their possible links to proxy risk factors. Inter-district differences in the geographic distribution of all breast cancers seemed to link breast cancer to different industrial and agricultural exposures between the districts. Interestingly, within district-level urban-rural differences, IBC cases were more likely to related to agricultural and industrial sites, sewage disposal, and other polluting sources that increase the levels of heavy metals contamination. Understanding the possible link between different geographic patterns of breast cancers and specific environmental exposures will need a further in-depth investigation of specific environmental factors to clarify the possible environmental risk factors of IBC in North Africa and elsewhere.
Acknowledgements
We are grateful to Mr. Khaled Daboos and other personnel of Gharbiah Cancer Society for their assistance throughout this project. We also would like to thank Mr. Kean McDermott for his technical assistance in Geographic Information System (GIS). An Nguyen was funded by the Cancer Epidemiology Education in Special Populations Program through funding from National Cancer Institute (USA) grant R25 CA112383.
References
- Ferlay J, Colombet M, Soerjomataram I, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. International Journal of Cancer. 2019; 144(8): 1941-1953. doi: 10.1002/ijc.31937.
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Ca : a Cancer Journal for Clinicians. 2018; 68(6): 394. doi: 10.3322/caac.21492.
- Hance KW, Anderson WF, Devesa SS, et al. Trends in inflammatory breast carcinoma incidence and survival: The surveillance, epidemiology, and end results program at the national cancer institute. J Natl Cancer Inst. 2005; 97(13): 966-975. doi: 10.1093/jnci/dji172.
- Levine PH, Veneroso C. The epidemiology of inflammatory breast cancer. Semin Oncol. 2008; 35(1): 11-16. doi: 10.1053/j.seminoncol.2007.11.018.
- Anderson WF, Schairer C, Chen BE, et al. Epidemiology of inflammatory breast cancer (IBC). Breast Disease. 2005; 22: 9-23.
- Boussen H, Bouzaiene H, Ben Hassouna J, et al. Inflammatory breast cancer in Tunisia: Reassessment of incidence and clinicopathological features. Semin Oncol. 2008; 35(1): 17-24. doi: 10.1053/j.seminoncol.2007.11.017.
- Boussen H, Bouzaiene H, Ben Hassouna J, et al. Inflammatory breast cancer in Tunisia. Cancer. 2010; 116: 2730-2735. doi: 10.1002/cncr.25175.
- Tamer MF, Naoto TU, Robert KY, et al. Distinct epidemiological profiles associated with inflammatory breast cancer (IBC): A comprehensive analysis of the IBC registry at the University of Texas MD Anderson Cancer Center. PLoS ONE. 2018; 13(9): e0204372. doi: 10.1371/journal.pone.0204372.
- Ismaili N, Elyaakoubi H, Bensouda Y, et al. Demographic, clinical, pathological, molecular, treatment characteristics and outcomes of nonmetastatic inflammatory breast cancer in Morocco: 2007 and 2008. Experimental hematology & oncology. 2014; 3(1): 1. doi: 10.1186/2162-3619-3-1.
- Soliman A, Spencer B, Khaled H, et al. Lower survival of inflammatory breast cancer in patients compared to survival of non-inflammatory breast cancer patients in Egypt. Cancer Res. 2009; 69.
- Scott L, Mobley LR, Il’yasova D, et al. Geospatial analysis of inflammatory breast cancer and associated community characteristics in the United States. International Journal of Environmental Research and Public Health. 2017; 14(4). doi: 10.3390/ijerph14040404.
- Le L, Schairer C, Hablas A, et al. Reliability of medical records in diagnosing inflammatory breast cancer in Egypt. Cancer Res. 2015; 75(15). doi: 10.1158/1538-7445.AM2015-5590.
- Schairer C, Hablas A, Eldein I, et al. Clinico-pathologic and mammographic characteristics of inflammatory and non-inflammatory breast cancer at six centers in North Africa. Breast Cancer Res Treat. 2019; 176(2): 407-417. doi: 10.1007/s10549-019-05237-5.
- International classification of diseases for oncology (ICD-O), 3d ed. Bull World Health Organ. 2001; 79(2): 179.
- Central Agency for Public Mobilization and Statistics. Egypt. 2006.
- Costa J, Webber BL, Levine PH, et al. Histopathological features of rapidly progressing breast carcinoma in Tunisia: A study of 94 cases. International Journal of Cancer. 1982; 30(1): 35-37. doi: 10.1002/ijc.2910300107.
- Dey S, Zhang Z, Hablas A, et al. Geographic patterns of cancer in the population-based registry of Egypt: Possible links to environmental exposures. Cancer Epidemiology. 2011; 35(3): 254-264. doi: 10.1016/j.canep.2010.09.010.
- Dey S, Soliman AS, Hablas A, et al. Urban–rural differences in breast cancer incidence in Egypt (1999–2006). The Breast. 2010; 19(5): 417-423. doi: 10.1016/j.breast.2010.04.005.
- Soliman AS, Vulimiri SV, Kleiner HE, et al. High levels of oxidative DNA damage in lymphocyte DNA of premenopausal breast cancer patients from Egypt. Int J Environ Health Res. 2004; 14(2): 121-134. doi: 10.1080/0960312042000209534.
- Awadallah RM, Soltan ME, Shabeb MSA, et al. Bacterial removal of nitrate, nitrite and sulphate in wastewater. Water Research. 1998; 32(10): 3080-3084.
- Abdel-Gawad S, Abdel-Shafy M. Pollution control of industrial wastewater from soap and oil industries: A case study. Water science and technology : a journal of the International Association on Water Pollution Research. 2002; 46(4-5): 77-82.
- Soltan ME, Awadallah RM. Chemical survey on the river Nile water from Aswan into the outlet. Journal of Environmental Science and Health .Part A: Environmental Science and Engineering and Toxicology. 1995; 30(8): 1647-1658. doi: 10.1080/10934529509376293.
- Shokr MS, El Baroudy AA, Fullen MA, et al. Spatial distribution of heavy metals in the Middle Nile Delta of Egypt. International Soil and Water Conservation Research. 2016; 4(4): 293-303. doi:10.1016/j.iswcr.2016.10.003.
- Ahmed S, Mazloum R, Abou-Ali H. Spatiotemporal interpolation of air pollutants in the Greater Cairo and the Delta, Egypt. Environ Res. 2018; 160: 27-34. doi: 10.1016/j.envres.2017.09.005.
- El-Kowrany S, El- Zamarany EA, El-Nouby K, et al. Water pollution in the Middle Nile Delta, Egypt: An environmental study. Journal of Advanced Research. 2016; 7(5): 781-794. doi: 10.1016/j.jare.2015.11.005.
- Ingram DD, Franco SJ. 2013 NCHS urban-rural classification scheme for the counties. National Center for Health Statistics. Vital Health Stat. 2014; 2(166).
- Anwar WA. Environmental health in Egypt. International J Hygiene & Env Health. 2003; 206: 339-50.
