Osteopoikilosis: Two Senegalese Case Reports
Moustapha Niasse1*, Baïdy Sy Kane2, Yetna Tcheindah1, Kaba Condé3, Coumba Diouf1, Léra Géraud Akpo4, Ibrahima Faye4, Saïdou Diallo1
1Department of Rheumatology, University Hospital Aristide Le Dantec of Dakar, Senegal
2Department of Internal Medicine, University Hospital Aristide Le Dantec of Dakar, Senegal
3Department of Rheumatology, University Hospital Ignace Deen of Conakry, Guinea
4Department of Radiology, University Hospital Aristide Le Dantec of Dakar, Senegal
Introduction
Osteopoikilosis (OPK) is a rare condensing benign bone osteopathy of unknown cause1, 2, 3. The first description of OPK dates from 1915, by Albers-Schönberg4, 5, 6. Both autosomal dominant and sporadic forms of OPK have been reported2, 3. Herein, we describe two Senegalese cases of this rare disease.
Observations
The first patient was a 35-year-old man who had consulted in April 2016 for mechanical pain that was localized in hips, feet, dorsal and lumbar spine. The clinical examination was normal. Standard radiography revealed diffuse condensing lesions. They were symmetrically distributed at periarticular locations, more frequently in the epiphysis and metaphysis of femur bones, tarsal bones, metatarsals, phalanges of feet and pelvic bones (figure 1). Thoracic, abdominal and pelvic CT scans showed the same lesions in the thoracic and lumbar spine (Figure 2). The CT scan did not show any evidence of cancer, such as breast, kidney, thyroid or lung cancers. Laboratory tests including blood count cells, C-reactive protein, erythrocyte sedimentation rate, serum calcemia, serum phosphorus were normal.

Figure 1: Standard radiography of the pelvis and feet: diffuse condensing lesions. They are symmetrically distributed in periarticular locations, more frequently in the epiphysis and metaphysis of femur bones (A), and tarsal bones, metatarsals, phalanges of feet (B) and pelvic bones (A).

Figure 2: Pelvic, dorsal and lumbar spine CT scans: radiographic images confirmed by CT scan (A). CT scan also found condensing lesions in the dorsal and lumbar spine (D11 to L3) and posterior joints (B).
The diagnosis of OPK was retained. The patient was reassured about the benign nature of the lesions, and received pain treatment. We did not research other cases of osteopoikilosis in our patient’s relatives.
The second patient was a 32-year-old woman. She consulted in September 2019 following a trauma of the right foot. The radiography of the feet and ankles unexpectedly found ovoid, symmetrical condensing lesions on the bones of the tarsus, metatarsus and phalanges (Figure 3). Complementary x-rays of the wrists and hands and pelvis detected the same lesions (Figure 3). Laboratory tests were normal as in the first case. The diagnosis of OPK was retained based on the the typical radiographic lesions. The patient was reassured about the benign nature of the lesions. We did not research other cases of osteopoikilosis in our patient’s relatives.
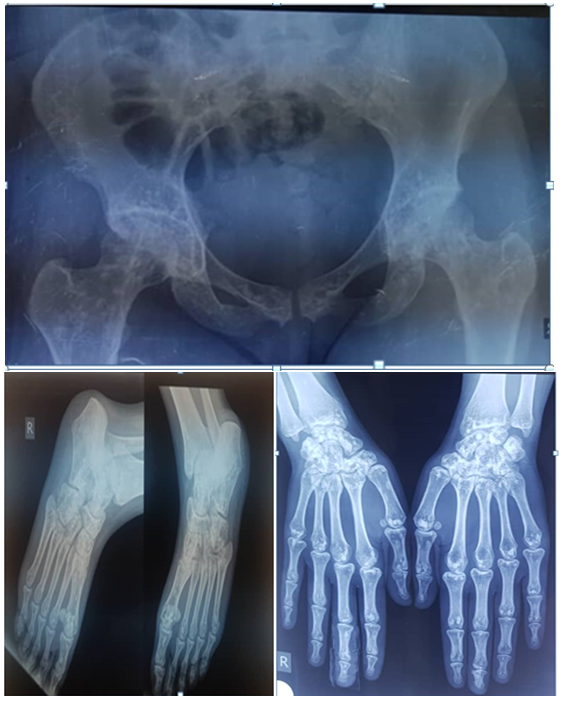
Figure 3: Standard radiography of the ankles and feet, wrists and hands and pelvis: diffuse condensing lesions. They are symmetrically distributed in periarticular locations, more frequently in the epiphysis and metaphysis of long tubular bones (A), carpal and tarsal bones, metacarpals, metatarsals, phalanges of hands and feet (B) and pelvic bones (A).
Discussion
Our 2 cases collected over a period of 3 years 06 months suggest a rarity of the disease in our context. OPK is a rare disease in any study population1, 2, 3, 3, 5, 7. The prevalence is estimated at 1/50000 in the Western population1, 2, 3. In the African literature, some observations have been reported, particularly in North Africa, notably in Morocco and Tunis 5, 8, 9, 10, 11. It is a disease that predominates in men with classic asymptomatic clinical expression3, 12, 13, but 15 to 20% of patients report joint pain and swelling3, 12, 14. In one of our patients the disease was revealed by osteo-articular pain while in the other, the discovery was incidental on X-ray images.
Radiologically, OPK lesions appear as sclerotic, numerous, well defined, homogenous, circular or ovoid, varying in size from a few millimeters to several centimeters. They are symmetrically distributed in periarticular locations, more frequently in the epiphysis and metaphysis of long tubular bones, carpal and tarsal bones, metacarpals, metatarsals, phalanges of hands and feet and pelvic bones13, 14, 15, 16. Involvement of other bone structures is less common and usually less marked13, 14. Lesions do not usually bind to bone scintigraphy13. Thus, the radiological description in our patients is in accordance with the data in the literature and the spinal involvement in the first patient is unusual.
OPK can be associated with several dermatologic manifestations, such as dermatofibrosis lenticularis disseminata (Buschke-Ollendorff syndrome), characterized by multiple papular fibromas on the back, arms, and thighs, or a predisposition to keloid formation, scleroderma-like lesions or discoid lupus erythematosus3, 14, 17, 18. According to some authors, OPK has been associated with other conditions such as dacryocystitis, heart or renal malformations and endocrine disorders, dental and facial anomalies as summarized by Gunal et al3, 19 and Sarralde et al3, 18. The association with other fibrous dysplasias such as melorheostosis, striated osteopathy or tuberous sclerosis is possible3, 14, 20. Current literatures suggest loss-of-function mutations of LEM domain containing 3 (LEMD3) gene located on 12q might be the cause, and the mutation could also affect soft tissue and skin, resulting in melorheostosis and Buschke–Ollendorff syndrome6, 21. In our patients, osteopoikilosis was not associated with other diseases.
It is therefore important to know the radiological semiology characteristic of this pathology in order to reassure the patient, to avoid investigations and unnecessary treatments13. However, surveillance of the disease is necessary because of the possibility of serious complications, including myelopathic ductal stenosis syndrome, retractile fibrosis and malignant degeneration3, 22, 23. The disease monitoring protocol is not well defined.
Conclusion
Osteopoikilosis is a rare disease. However, our two observations confirm its existence in our practice. The diagnosis is based on typical radiographic lesions and normal biological tests. It is a benign disease, but it must be monitored because of possible risk of malignant degeneration.
References
- Madeira N, Ganhão S, Ferreira RM, et al. Osteopoikilosis: case series from Portuguese Rheumatology centers. Acta Reumatol Port. 2019; 44: 78-83.
- Butkus CE, Michels VV, Lindor NM, et al. Melorheostosis in a patient with familial osteopoikilosis. Am J Med Genet. 1997; 72: 43-46.
- Borman P, Özoran K, AydoÄ S, et al. Osteopoikilosis: report of a clinical case and review of the literature. Joint Bone Spine. 2002; 69: 230-233.
- Negi RS, Manchanda KL, Sanga S, et al. Osteopoikilosis – spotted bone disease. Med J Armed Forces India. 2013; 69: 196-198.
- Mahbouba J, Mondher G, Amira M, et al. Osteopoikilosis: A rare cause of bone pain. Caspian J Intern Med. 2015; 6(3): 177-179.
- Tsai SY, Wang SY, Shiau YC, et al. Benign incidental findings of osteopoikilosis on Tc-99m MDP bone SPECT/CT A case report and literature review. Medicine. 2016; 95: 23.
- Diallo Saïdou, Diouf Coumba, Niasse Moustapha, et al. What is your diagnosis? Rev Mar de Rhum. 2017; 39: 65-66.
- Haddad N, Hila A, Amri H, et al. Familial osteopoikilosis in a diabetic. Tunis Med. 1976; 54(4): 667-673.
- Zahar A, Najeb Y, Rafai M, et al. Femoral neck fracture in osteopoikilosis. Rev Chir Orthop Reparatrice Appar Mot. 2002; 88(7): 725-727.
- Laurenti. On a case of osteopoecilia. Tunis Med. 1955; 43(10): 1009-1013.
- Laurenti J, Teman H. Family osteopoecilia. Tunis Med. 1956; 34(9): 831.
- Korkmaz MF, Elli M, Özkan MB, et al. Osteopoikilosis: report of a familial case and review of the literature. Rheumatol Int. 2015; 35(5): 921-924.
- Desmots F, Gabaudan C, Geffroy Y. Osteopoikilosis : a « no touch lesion ». Feuillets de radiologie. 2011; 51: 284-285.
- Bachmeyer C, Langman B, Danon O, et al. Benign sclerotic lesions: osteopoikilosis. Presse Med. 2007; 36: 1212-1213.
- Belkhou A, Ajrinija A, El Hadrami Z, et al. Osteopoikilosis. Feuillets de radiologie. 2014; 54: 394-395.
- Al-Bourini O, Lotz J, Wienbeck S. Radiological Findings in Osteopoikilosis. Rofo. 2018; 190(6): 499-502.
- Hassikou H, Tabache F, Safi S, et al. Buschke–Ollendorff syndrome. Revue du Rhumatisme. 2008; 75: 292-294.
- Diociaiuti A. Buschke–Ollendorff syndrome. British Journal of Dermatology. 2016; 174: 709-722.
- Gunal I, Seber S, Basaran N, et al. Dacryocystitis associated with osteopoikilosis. Clin Genet. 1993; 44: 211-213.
- Gnoli M, Staals EL, Campanacci L, et al. Melorheostosis and Osteopoikilosis Clinical and Molecular Description of an Italian Case Series. Calcif Tissue Int. 2019; 105(2): 215-221.
- Zhang Q, Mo ZH, Dong CS, et al. Identification of a novel LEMD3 Y871X mutation in a three generation family with osteopoikilosis and review of the literature. J Endocrinol Invest. 2016; 39(6): 679-685.
- Sarralde A, Garcia-Cruz D, Nazara Z, et al. Osteopoikilosis: a report of a familial case. Genet Counsel. 1994; 5: 373-375.
- Walpole IR, Manners PJ. Clinical considerations in Buschke-Ollendorff syndrome. Clin Genet. 1990; 37: 50-63.
